The Stages Before and After Stroke – SyreboCare
A stroke happens when the blood supply to the brain is interrupted. In about 80% of cases, this happens because of a blood clot or blocked artery. Strokes can also happen if the blood vessel itself is damaged. Without a good blood supply, the brain cells don’t get the oxygen they need to function. If the supply is interrupted for long enough, the brain cells will die.
The effects of a stroke will depend on how long the interruption lasts. A mini-stroke or transient ischemic attack (TIA) happens when the blood vessel is just temporarily blocked. The symptoms can go away within minutes as the blood supply returns and there might not be much permanent damage to the brain cells. A TIA can be a sign that a more serious stroke is on the way, so it is important to take them seriously and to seek help, even if the symptoms go away by themselves. About 4 in 10 people who have a TIA will go on to have a stroke
What happens days before a stroke?
The signs of a stroke often appear suddenly, but that doesn’t mean that you won’t have time to act. Some people will experience symptoms such as headaches, numbness or tingling several days before they have a serious stroke. One study found that 43% of stroke patients experienced mini-stroke symptoms up to a week before they had a major stroke.
There are some possible symptoms that you should watch out for too:
- A sudden, severe headache
- Sudden dizziness, loss of balance or coordination
- Loss of vision or changes to your vision in one or both eyes, which usually happen suddenly
- Feeling confused or having trouble understanding things that are usually easy for you
- Numbness or weakness on one side of the body (or in one arm or leg)
If you take note of these symptoms and seek help even if they go away, then your chances of a good recovery are much better. Don’t ignore the early warning signs. You aren’t overreacting if there’s a change; you’ve had a TIA. Get help right away as a more serious stroke could be hours or days away.
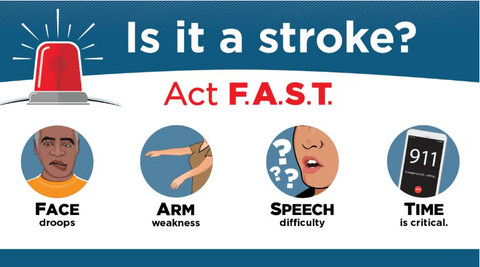
You might have heard the FAST acronym before. It’s an easy way to remember the most common warning signs of a stroke and the importance of acting quickly:
- Face drooping (if you ask them to smile then it will be crooked or one-sided)
- Arm weakness or numbness (if you ask them to lift both arms, one will drop lower than the other)
- Speech problems such as slurring or difficulty repeating a sentence
- Time to call an ambulance
What are the 7 stages after a stroke?
By understanding the stages of stroke recovery, stroke survivors and their families will have a clearer understanding of what to expect during the recovery process. Knowing that recovery typically progresses through stages can reduce patients’ anxiety and frustration by setting realistic expectations for improvement over time.
Stage One: Flaccidity
The first stage immediately after a stroke is flaccidity. This is where the muscles on the affected side of the body are completely limp and unable to move. Nerve damage in the brain means that there are no voluntary movements.
The best way to help at this stage is to assist with passive movement. The stroke victim themselves are likely to be able to use the mobile side of their body to passively move the flaccid side; it’s important to encourage this. It may not seem like it’s doing much but it is increasing sensory input to the brain by sending signals from skin and muscle about movement and touch. These actions will encourage that side of the brain to start waking up.
At this stage, passive movement can also help prevent atrophy. If long term paralysis does take place this can cause the muscle to start to wither and the overall rehabilitation will be more difficult, so the muscles need to receive some form of stimulation. It is also good for the joints and tendons to experience regular movement.
Stage Two: Spasticity
The second stage of stroke recovery is the appearance of muscle stiffness and rigidity (spasticity).
At rest, the patient's limbs may stay contracted (usually in a "flexed" position, with the elbow and wrist bent), or they may jerk or tremble when the patient tries to move them. The patient may have some voluntary movement back at this point, but not much.
Spasticity happens as the brain starts to rebuild connections with the muscles.
In a way, spasticity is sort of a positive thing. However, the connection is incomplete at this stage of stroke recovery, which is why the muscles can get "stuck" in contracted positions or not move in the way the patient wants them to.
Stage Three – Spasticity Increases
In the third stage of stroke recovery, spasticity increases. This can be frustrating and stroke patients may feel that they are getting worse and not moving forward in their stroke recovery.
Try to remember that the increase in spasticity is positive, even if it doesn't feel like it. The patient's brain is still working to rebuild connections with their muscles.
During this stage of stroke recovery, the patient will continue with and progress in your therapeutic exercises. The patient will likely focus on performing as much active movement as possible, although this will be challenging.
Stage Four – Spasticity Decreases
In the fourth stage, spasticity starts to decrease. This is a big milestone in the stroke recovery process.
As spasticity decreases, stroke patients will notice improved voluntary movement patterns, but their movements will still feel jerky, twitchy, and uncoordinated.
With the remaining spasticity, stroke patients may still have trouble releasing objects. For example, a stroke patient might be able to grasp a fork but be unable to let go of it.
Stroke patients will likely still be very weak from the lack of voluntary movement in the first three recovery stages of stroke recovery. Working on range of motion, stretching and weight-bearing exercises should be focused on.
In this regard, hand exercise tools such as rehabilitation gloves can help patients immensely. Learn more.
Stage Five – Return of Complex Movement
More and more signals from the brain to the muscles will be successful, and involuntary movements will be minimal. At this stage complex actions like using cutlery, writing, walking and swimming can all be achieved through movement repetition.
At this stage, stroke patients will have regained most of their movement, so they will want to strengthen their muscles back to how they were pre-stoke. This can be done by adding small weights or resistance bands to previous rehabilitation exercises.
Stage Six – Spasticity Disappears
At this stage, there will be no unexpected involuntary movements, and coordination will quickly improve.
Stroke patients should continue strengthening their muscles and focus on fine-tuning their motor skills with activities such as drawing, playing an instrument, shuffling cards or any other hobby they used to have pre-stroke.
Stage Seven – Return to Normal
In the seventh and final stage of stroke recovery, stroke patients' normal function returns.
Stroke patients can now perform complex, coordinated, synergistic movement patterns on their affected side as well as on their unaffected side. Patients can return to their meaningful occupations with independence.
While this stage is the big goal for patients, not everyone will reach this stage after having a stroke.
Summary
Stroke recovery is unique to each person. However, most providers assess progress using seven stages of stroke recovery, which include the following: flaccidity, spasticity appears, spasticity increases, spasticity decreases, complex movement combinations, spasticity disappears, and normal function returns.
How long it takes a person to move through the stages of stroke recovery and how many stages they successfully make it through varies. Other factors like overall health, socioeconomics, and the type and severity of the stroke affect recovery. However, the use of quality hand exercise tools will certainly have a positive impact on the patient's mobility recovery.
Keep in mind that even years after a stroke, people can achieve meaningful stroke recovery because the brain can keep adjusting and changing. To learn more about stroke, click here.








